Minimally invasive spinal surgery (MISS) is transforming spine care, offering a less disruptive approach compared to traditional open surgery. For many, it can lead to quicker recoveries and reduced risks. For many patients suffering from back pain, herniated discs, or other spine-related issues, this approach has proven to be a highly effective solution. Dr. Larry Davidson, a respected name in spinal surgery, highlights that advancements in MISS have provided patients with safer, more targeted treatment options.Just what do patients need to know about minimally invasive spinal surgery?
The Benefits of Minimally Invasive Spinal Surgery
For patients exploring their options, the benefits of MISS are a major consideration. Compared to traditional open spinal surgery, minimally invasive techniques are designed to limit tissue damage, reduce blood loss and minimize postoperative pain. Because of these advantages, many patients can experience shorter hospital stays and quicker recoveries, helping them return to daily activities with less downtime.Additionally, the potential for lower complication risks, such as infections, may be especially beneficial for those with existing health conditions, making MISS a strong consideration for many.
Beyond physical benefits, patients often report improved emotional and mental well-being during recovery. Shorter recovery periods mean less time off work, fewer disruptions to daily routines and overall reduced stress, contributing to an enhanced quality of life.
Common Procedures in Minimally Invasive Spinal Surgery
Minimally invasive spinal surgery is used to treat a wide range of spinal conditions, from degenerative disc disease to spinal stenosis. Some of the most performed procedures include:
Microdiscectomy: Often recommended for herniated disc treatment, this procedure involves removing a small section of the disc or bone material compressing spinal nerves. With minimal disruption to surrounding tissues, patients usually experience immediate relief from symptoms and can resume daily activities faster than with open surgery.
Spinal Fusion: Used to stabilize vertebrae in cases of severe degeneration or injury, minimally invasive spinal fusion reduces the size of the incision and preserves more of the muscle tissue than open surgery. This technique is especially helpful in treating chronic back pain, restoring stability and enhancing spinal function.
Laminectomy and Foraminotomy: These procedures focus on creating more space within the spinal canal to relieve pressure on nerves. MISS techniques allow surgeons to remove only the necessary portions of bone or tissue, preserving stability while reducing recovery time. P Patients with spinal stenosis may benefit from these procedures, potentially regaining mobility and experiencing reduced symptoms.
How Minimally Invasive Spinal Surgery Works
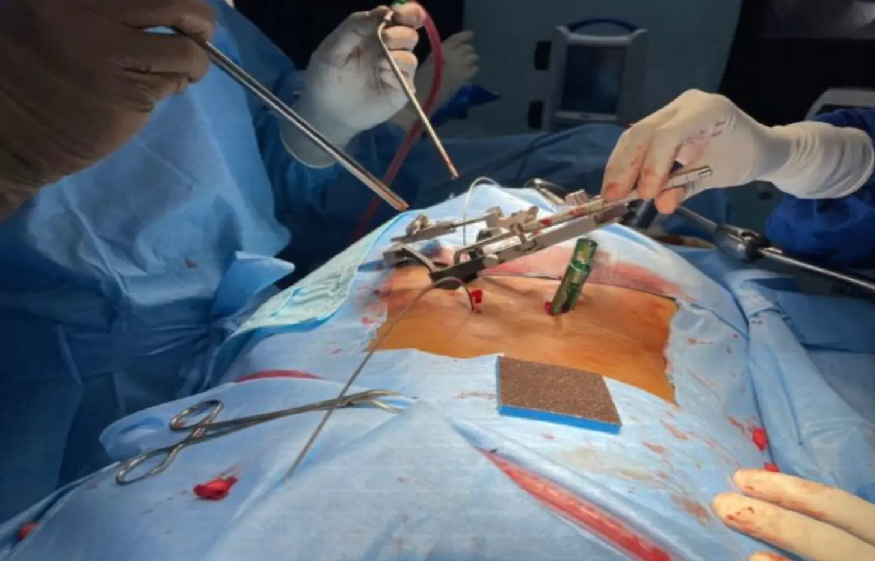
The MISS approach is based on advanced surgical tools and technology, allowing surgeons to operate with extreme precision. Most procedures utilize a tubular retractor, which enables surgeons to create small incisions and reach affected areas without cutting through large amounts of muscle or other tissues. Tiny cameras, known as endoscopes, are used to guide the surgeon, ensuring that they can see and operate accurately with minimal impact on the surrounding anatomy.
This technique differs significantly from traditional surgery, which typically requires larger incisions to access the spine. By aiming to reduce tissue disruption, MISS may support faster recoveries, reduced postoperative discomfort and a lower likelihood of complications, making it a valuable option for eligible patients. The integration of robotic assistance in MISS has also enhanced outcomes, allowing surgeons to perform procedures with even greater accuracy and control, ensuring positive results for complex cases.
Recovery and Postoperative Expectations
One of the most significant advantages of MISS is the shorter recovery period. Patients may be able to go home on the same day or within a few days of surgery, depending on the specific procedure and their overall health. Recovery times are shorter, with many patients able to resume light activities within a few weeks, gradually progressing to full mobility as advised by their healthcare team.
However, patients must follow all postoperative care instructions to optimize recovery. This typically includes:
Physical Therapy: Gradual exercises and physical therapy play a vital role in rebuilding strength, flexibility and stability in the spine. Physical therapists create customized routines that target specific muscles and promote safe movement, helping patients regain mobility and prevent future injuries.
Pain Management: MISS typically results in less pain than open surgery, but some discomfort can still occur. Doctors may prescribe medication or recommend non-drug options like ice, heat and gentle stretching. For some MISS patients, over-the-counter medications may be sufficient to help manage discomfort without the need for stronger drugs.
Follow-up Appointments: Regular check-ups allow surgeons to monitor healing progress and address any concerns. These appointments are crucial for identifying and managing potential complications early on, ensuring that the patient’s recovery stays on track. In some cases, additional imaging studies, like X-rays or MRIs, may be used to confirm proper healing.
Risks and Considerations of Minimally Invasive Spinal Surgery
Although MISS has a high success rate, no surgery is entirely without risks. While complications are uncommon, there is a possibility of issues such as infection, nerve irritation, or limited symptom relief. Patients are encouraged to discuss these potential risks with their healthcare providers to make a well-informed decision. Patients should discuss these potential risks with their healthcare providers to make an informed decision. Specialists often recommend that patients fully understand both the benefits and risks of MISS compared to traditional surgery to make the choice that best suits their lifestyle and medical needs.
MISS may not be suitable for all patients. In cases of severe spinal deformities, significant scoliosis, or extensive damage, traditional open surgery may be a more appropriate choice. Factors such as age, overall health status and lifestyle can also influence a patient’s eligibility for MISS. Consulting with a spinal specialist can provide clarity, allowing patients to consider all options and understand the rationale for choosing one approach over another.
Is Minimally Invasive Spinal Surgery Right for You?
Minimally invasive techniques provide an appealing alternative for patients considering spinal surgery, but they are not universally suitable. A thorough assessment with a qualified spinal surgeon like Dr. Larry Davidson can help to determine the most appropriate course of action based on individual circumstances. Patients are encouraged to ask questions, seek second opinions if needed and thoroughlyreview all options, as understanding the treatment’s benefits and limitations is crucial to making an informed choice.
Transforming Spine Care with Minimally Invasive Approaches
Minimally invasive spinal surgery represents a significant advancement in modern spine care, offering effective treatment options with reduced recovery times and less postoperative pain. For many patients, this innovative approach provides relief from chronic pain, improves quality of life and limits the physical impact of surgery. Minimally invasive spinal surgery can be a valuable optionfor immediate symptom relief or long-term spinal health. Consulting with an experienced spinal specialist is the first step toward making an informed, personalized decision about spine health.